bFGF blockade reduces intraplaque angiogenesis and macrophage infiltration in atherosclerotic vein graft lesions in ApoE3*Leiden mice
Intraplaque angiogenesis increases the chance of unstable atherosclerotic plaque rupture and thrombus formation leading to myocardial infarction. Basic Fibroblast Growth Factor (bFGF) plays a key role in angiogenesis and inflammation and is involved in the pathogenesis of atherosclerosis.
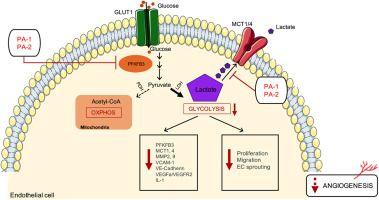
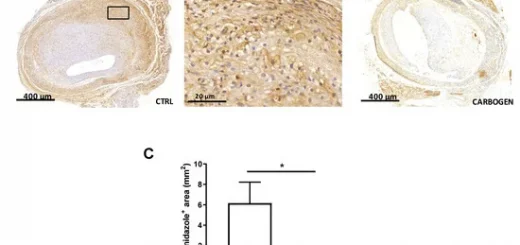
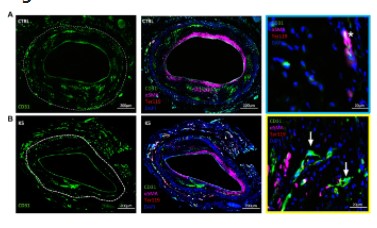
Therefore, we aim to test K5, a small molecule bFGF-inhibitor, on remodelling of accelerated atherosclerotic vein grafts lesions in ApoE3Leiden mice. K5-mediated bFGF-signalling blockade strongly decreased intraplaque angiogenesis and intraplaque hemorrhage. Moreover, it reduced macrophage infiltration in the lesions by modulating CCL2 and VCAM1 expression. Therefore, K5 increases plaque stability. To study the isolated effect of K5 on angiogenesis and SMCs-mediated intimal hyperplasia formation, we used an in vivo Matrigel-plug mouse model that reveals the effects on in vivo angiogenesis and femoral artery cuff model to exclusively looks at SMCs. K5 drastically reduced in vivo angiogenesis in the matrigel plug model while no effect on SMCs migration nor proliferation could be seen in the femoral artery cuff model. Moreover, in vitro K5 impaired endothelial cells functions, decreasing migration, proliferation and tube formation. Our data show that K5-mediated bFGF signalling blockade in hypercholesterolemic ApoE3Leiden mice reduces intraplaque angiogenesis, haemorrhage and inflammation. Therefore, K5 is a promising candidate to stabilize advanced atherosclerotic plaques.